The first blood biomarker to distinguish between myocarditis and acute myocardial infarction
miR-72 is a novel marker to distinguish between myocarditis and acute myocardial infarction
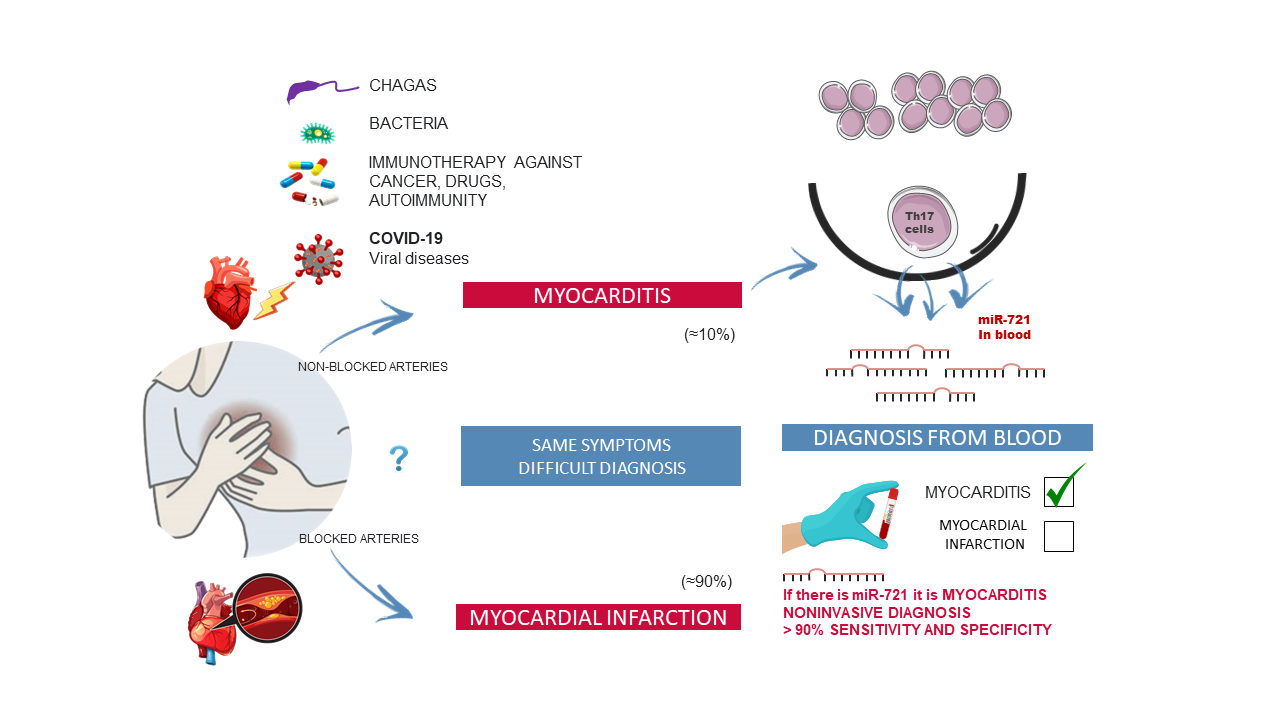
Scientists at the Centro Nacional de Investigaciones Cardiovasculares (CNIC) have identified the first blood biomarker for myocarditis, a cardiac disease that is often misdiagnosed as myocardial infarction. The new finding is especially pertinent now because myocarditis is a possible complication of COVID-19. Studies suggest that myocarditis may affect around 30% of COVID-19 patients hospitalized with acute respiratory syndrome and elevated troponins. Nevertheless, the diagnosis of myocarditis continues to be challenging in clinical practice. The study, led by Dr. Pilar Martín and published today in The New England Journal of Medicine, has detected the presence of the human homolog of micro RNA miR-721 in the blood of myocarditis patients. CNIC General Director Dr. Valentín Fuster emphasizes that these results of paramount importance because they establish the first validated blood marker with high sensitivity and specifity (>90%) for myocarditis. This will allow clinicians to distinguish between this disease and other cardiomyopathies like acute myocardial infarction, myocardial infarction with nonobstructive coronary arteries (MINOCA), and other inflammatory diseases with an autoimmune origin. “Our finding has great potential as a valuable clinical tool for the precise and noninvasive diagnosis of myocarditis from small drops of blood,” says Dr. Martín, whose project is funded by a Fundación BBVA Beca Leonardo award. The diagnosis of myocarditis is challenging, and the availability of a sensitive and specific marker of acute myocardial inflammation could have a major clinical impact, improving the diagnosis of myocarditis both generally and particularly in its early phases.
An inflammatory disease of the heart
Myocarditis is an inflammatory disease of the heart caused by infection, toxins, drugs, or autoimmune disorders. If untreated, myocarditis can progress to potentially fatal dilated cardiomyopathy, requiring heart transplant. The prevalence of myocarditis remains uncertain because it is often difficult to achieve a confirmed diagnosis. Myocarditis, says study co-first author Rafael Blanco-Domínguez, “is often the final diagnosis in patients with MINOCA, which accounts for 10-20% of patients meeting the criteria for myocardial infarction.” Myocarditis is usually diagnosed after coronary angiography or computed tomography scans have discarded coronary artery disease, followed by confirmation of the diagnosis by magnetic resonance imaging (MRI). However, not all centers have access to MRI technology, and the current gold standard for myocarditis diagnosis is endomyocardial biopsy, an invasive procedure normally reserved for severe cases. There is thus a pressing clinical need for the development of reliable and accessible tools for the early diagnosis of acute myocarditis. The most frequent cause of myocarditis is viral infection. Pilar Martín notes that “myocarditis can be one of the clinical presentations or complications of patients with COVID-19, the disease caused by the coronavirus SARS-CoV-2. The data suggest that myocarditis may affect around 30% of hospitalized COVID-19 patients with severe acute respiratory syndrome and elevated troponins, thus representing an emerging clinical problem.” This context underlines the need for a valid biomarker of myocarditis, since the magnitude of the COVID-19 pandemic precludes long-term follow-up of all patients by MRI or endomyocardial biopsy. “We need new biomarkers to assess these patients and the association between myocarditis and progression to dilated cardiomyopathy and other adverse cardiac events,” says Pilar Martín. This is especially relevant to the situation of professional athletes who have had COVID-19, because competitive sport can aggravate this disease worsen and its prognosis. Moreover, adds Raquel Sánchez-Díaz, “myocarditis is the most lethal secondary effect of cancer therapy with new immune checkpoint inhibitors. Among cancer patients treated with these drugs who develop myocarditis, half die.” There are currently no specific markers for the diagnosis of patients susceptible to developing myocarditis during cancer immunotherapy. “We identified miR-721 in the blood plasma of mice with autoimmune or viral myocarditis. This miRNA is produced by autoimmune Th17 cells that recognize cardiac antigens derived from proteins such as alpha-myosin,” says Rafael Blanco-Domínguez. Continuing, study co-first author Raquel Sánchez-Díaz explains that “these cells attack the myocardium, and are in large part responsible for the pathophysiology of the disease.” The research team went on to identify, clone, and validate the previously unknown human homolog of miR-721. The study confirmed that this miRNA is synthesized in the Th17 cells of myocarditis patients and its expression is exclusively detected in the plasma of these patients. The biomarker was validated by cardiologists and researchers at numerous hospitals in Spain and abroad. In Spain, key contributors include Drs. Francisco Sánchez-Madrid, Hortensia de la Fuente, Jesús Jiménez-Borreguero, Fernando Alfonso, Isidoro González, and Esteban Dauden of Hospital de la Princesa; Dr. Valentín Fuster of the CNIC, Dr. Borja Ibáñez of Fundación Jiménez Díaz and the CNIC; Dr. Héctor Bueno of Hospital Doce de Octubre; Dr. Amaia Martínez of Hospital Central de Asturias; Dr. Leticia Fernández Friera of HM Montepríncipe; Dr. Domingo Pascual-Figal of Hospital Virgen de la Arrixaca, and Dr. Villar Guimerans of Hospital Ramón y Cajal. Key international contributors include the University of Padua in Italy, Zürich University Hospital in Switzerland, and Massachusetts General Hospital and the Mayo Clinic in the USA.
The researchers are currently designing studies to evaluate the potential of the biomarker as a predictor of short-term and long-term risk, the persistence of myocardial inflammation, and the risk of relapse, clinical progression, and adverse ventricular remodeling. The CNIC is the sole owner of a patent related to the biomarker and its use for the diagnosis of miocarditis. The CNIC is now exploring licensing agreements with industrial partners to develop and commercialize this technology in order to make it available for clinical use. For Dr. Fuster, “this study is a shining example of how the basic research carried out at the CNIC contributes to societal wellbeing through the translation of the knowledge gained in the center’s laboratorios to clinical practice.” The study received funding from the Ministerio de Ciencia e Innovación (MICINN) through the Instituto de Salud Carlos III (ISCIII)-Fondo de Investigación Sanitaria; the CIBERCV; the Comunidad de Madrid; a Fundación BBVA Beca Leonardo award; Fundació La Marató TV3; and European Research Council grants ERC-2011-AdG 294340-GENTRIS to F.S-M. and ERC-2018-CoG 819775-MATRIX to B.I.
About the CNIC
The Centro Nacional de Investigaciones Cardiovasculares (CNIC), directed by Dr. Valentín Fuster, is dedicated to cardiovascular research and the translation of knowledge gained into real benefits for patients. The CNIC, recognized by the Spanish government as a Severo Ochoa center of excellence, is financed through a pioneering public-private partnership between the government (through the Carlos III Institute of Health) and the Pro-CNIC Foundation, which brings together 12 of the most important Spanish private companies.
Information and interview requests
Fátima Lois: CNIC Head of Communications. flois@cnic.es / Tel 639282477
Rafael Ibarra: CNIC Communications Office. ribarra@cnic.es / 914531200. Ext 4232